The need for organ transplants is growing at a rate that needs to be urgently addressed
In 2016, 18 of every 100,000 Canadians needed an organ transplant. Of these 6,700 individuals, 260 died waiting for transplants, 409 withdrew from the list, 3,135 went into 2017 awaiting a transplant and 2,903 (43%) were fortunate enough to receive an organ. In the USA it’s a different story, where 95% of the adult population supports organ donation, yet only 54% are signed up as donors. Of donors, it’s likely that only 3 in 1000 deaths will be capable of donating organs, and the need for organ donation increases every 10 minutes. In 2017, UNOS reported 114,964 US individuals requiring lifesaving organ transplants, 16,464 (37.6% from living donors) generous donations were made, providing 34,769 transplants (23% of the waiting list). As of this blog, 1.7% of those on the UNOS list are under 18 years, and 31% are between the young ages of 18 to 49. It appears current organ donation practices aren’t sufficient to meet society’s needs.
Organ transplants on an Ag blog?
This may not seem like the appropriate forum to discuss organ donation policies, but I disagree. As a reader, you aren’t without the risk of potentially needing an organ. It is likely that you know someone who has or will be dramatically impacted by needing an organ transplant. Human to human donation is vital, however, it’s not enough, xenotransplantation may be an option we have to consider.
Xenotransplantation
The term xenotransplantation (aka xenograft) refers to a human recipient of a non-human animal in the form of living cells, tissue, or organ. The medical field has already turned to animals for soft tissue transplants. Porcine (pig) heart valve replacements have been used for years as replacements with synthetic/mechanical a more recent options. The skin of fish such as tilapia has been recently introduced as grafts for burn-victim treatments. Not to mention the breakthrough of New Zealand firms, Living Cell Technologies and Diatranz Otsuka Limited that created a pig islet therapy which is used to treat type 1 diabetes. After a successful 10 year clinical trial and ongoing patient survival, they have licensed DIABECELL®in both the USA and Japan.
Soft tissue transplants and grafts from animals have increased, while solid organ grafts or transplants are more difficult. Despite humans being closely related to chimpanzees, porcine organs are preferred for donation. The reason being that they are both similar in size and function to humans, plus the shorter growth time and larger litters make it more economical. The downside of pig organ donations are concerns of organ rejection due to pig-to-human immunological capability and the risk of transmitting porcine endogenous retrovirus (PERVs). Fortunately, it appears that both concerns can be addressed through gene editing (GE).
Gene editing medical research
Numerous groups of researchers are seeking to prevent the transmission of PERVs[1] such as eGenesis and the Harvard Medical School through the use of the genomic editing tool CRISPR–Cas9. eGenesis has successfully edited PERVs out of the pig genome in all 62 locations using CRISPR-Cas9, reducing the likelihood of transmission 1000 fold. Potentially, GE technology can be utilized for organ xenotransplantation to reduce the risk of PERVs transmission, causing rejection.
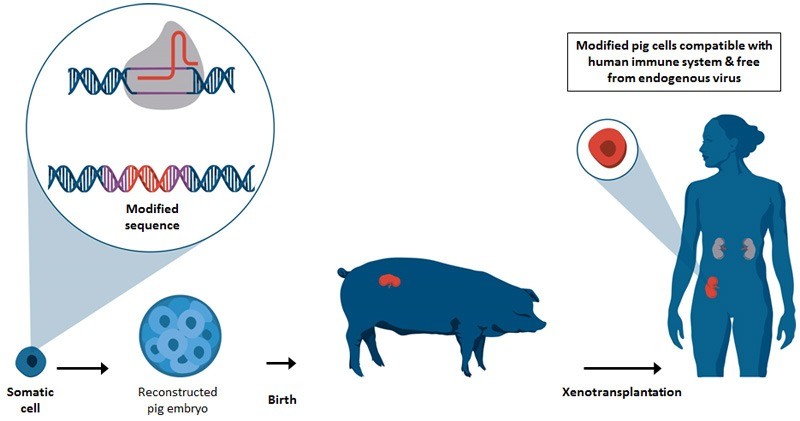
CRISPR-Cas9 cell edits for xenotransplantation organ donation
Stem cell research through CRISPR-Cas9 can also open opportunities for using an animal as a surrogate to grow your own custom organ for transplant. Both stem cell research and GE science are contentious topics, but we shouldn’t ignore the ability to produce human organs within another host for a perfect donation match.
From farm to the operating room?
If regulators approve the GE medical marvels of organ production, farming could expand into the medical field. Specialized medical farms might produce medical grade porcine organ donations. Farmed organs could allow organ recipients to start immunologic treatments ahead of surgery to reduce the chance of rejection. Not to mention patients would receive a healthy organ harvested at the optimum time. Farmed organs could reduce rejection, waiting times and the continued degradation of the patients’ health. There is a continual shortage of viable human organ donations meaning an expected 60% of patients on the wait list will die. If organs can be successfully donated from pigs, they can be used to save a life, or bridge the patients’ treatment until they can receive a human or mechanical organ. Farming organs might sound questionable, but if it could save lives, why would it be any different than producing animals for food?
The ethics of xenotransplantation
These new organ transplant research options open a host of ethical uncertainties. It’s unknown if farmed organs will become a long-term solution to organ transplant or whether they’ll be allowed. What is apparent is the need for a solution, and currently, xenotransplantation is pushing science to seek new solutions. As science pushes for a solution it’ll be society, industry and regulatory bodies’ responsibility to question the ethics of animal welfare, human acceptance and intervention.
What is society willing to accept and where will we draw the line? Is it more ethical relying on a constant supply of animal farmed organs or the small sample of harvestable organs from brain-dead cadavers? Due to being non-human organs and from GE science, will society railroad this as an optimal solution to our organ shortage?
At what time is it acceptable to allow xenotransplantation? Will it be permitted as a last resort, or will it be based on the alternate cost of medical care? The Canadian Institute for Health Information calculated (excluding in Quebec), Canada spends 1.1% of its total yearly health expenditure ($1.9 billion) on dialysis alone, which in 2014 accounted for 20,690 patients suffering from end-stage kidney disease. With such high costs to health care and diminished quality of life and expectancy, the idea of medical farms and organ donation may be less of an ethical concern.
Agriculture needs to determine where they stand
At the end of the day, from an agriculture and science perspective, we must first ask if raising animals for human organ donation is ethical. Once this has been determined, science must either step back from such practices or continue to invest in research. Ultimately, it will be society’s choice to accept such practices and give medical agriculture a chance to help save lives.
[1] PERVs is the result of a sugar and protein molecule found on the surface of porcine cells which humans don’t have. The introduction of these molecules to humans are foreign, causing the human’s body to react and potentially reject the new organ or tissue.
While xenografting is a possibility for the future, it not a solution we can use today for organ transplants. Until then, those among the transplant waiting list are still in need of organ donation and finanical support. If you would like to learn more about how you can generously donate or plan for donation click:
[su_button url=”https://www.canada.ca/en/public-health/services/diseases/blood-organ-tissue-donation.html#map-container” target=”blank” style=”glass” background=”#ed0009″ size=”5″ radius=”round” icon=”icon: heart” icon_color=”#ffffff” text_shadow=”0px 0px 0px #000000″]To learn about blood, organ and tissue donations across Canada[/su_button]
[su_button url=”https://unos.org/donation/” target=”blank” style=”glass” background=”#002eed” size=”5″ radius=”round” icon=”icon: heart” icon_color=”#f70909″ text_shadow=”0px 0px 0px #000000″]or learn about donations in the USA[/su_button]